It was his thing as a neuroscientist-physician. He developed one for Alzheimer’s disease and was on his way to developing one for amyotrophic lateral sclerosis (ALS), the disease he had been studying even before he got sick with it.
In reality, he had declined significantly since his diagnosis of ALS two years prior. First, he lost his speech, then his mobility, and very quickly breathing became a struggle. But any talk of the decline came with an acceptance that his life was imminently finite, and neither of us was willing to accept that outcome.
But Rahul did die, six months after that conversation.
What is ALS?
Amyotrophic lateral sclerosis (ALS), often known as Lou Gehrig’s disease or motor neuron disease, is a progressive degenerative disease in which nerve cells that mediate voluntary muscular movement are destroyed.
Motor neurons control movement in the arms, legs, chest, throat, and mouth. They run from the brain through the brainstem or spinal cord to muscles that control movement in the arms, legs, chest, throat, and mouth. These cells die in persons with ALS, causing muscular tissue to fade away.
ALS has no effect on a person’s sensory or mental abilities.
In general, there are two classifications for ALS: Lower motor neuron illness affects nerves that originate in the spinal cord or brainstem, while upper motor neuron disease affects nerves in the brain. Motor neurons are injured in both situations and eventually die. ALS is a deadly disease.
After a diagnosis, the typical life expectancy is two to five years, however some people can live for years or even decades. (For example, famed physicist Stephen Hawking lived for more than 50 years after being diagnosed with cancer.) There is no known treatment or cure for ALS.
A distinct proportion of upper and lower motor neurons die in each person with ALS. Symptoms differ from person to person as a result of this.
The condition worsens with time, impacting more nerve cells. Muscles weaken and atrophy (wither) as muscular tissues degrade, and the person’s limbs may appear thinner.
Muscles can also become spastic (move involuntarily), which can result in increased muscular tone in certain areas of the body.
What are the symptoms of ALS?
The initial symptoms of ALS can vary considerably from person to person, as can the rate at which ALS progresses. Not all individuals with ALS develop the same symptoms or the same sequences or patterns of progression. However, all people with ALS will experience progressive muscle weakness and paralysis.
In the early stages of ALS, the symptoms may be so minor that they are overlooked. Common symptoms include:
- Weakness in muscles of the hands, arms or legs
- Impairment in the use of arms and legs
- Twitching and cramping of muscles, especially those in the hands and feet
- Weakness in the muscles that control speech, swallowing or breathing
- Slow or slurred speech (called dysarthria or “thick speech”) and difficulty in projecting the voice
In more advanced stages, ALS causes shortness of breath and difficulty in breathing and swallowing, which is what eventally lead to a person’s death.
Who gets ALS?
In the United States, about 60% of those diagnosed with ALS are men, and 93 percent of patients are Caucasians. According to US demographic statistics, about 5,600 persons in the United States are diagnosed with ALS each year, or about 15 new cases every day. At any given time, it is estimated that up to 30,000 Americans are infected with the disease.
The majority of patients with ALS develop it between the ages of 40 and 70, with an average age of 55 at diagnosis. Rare incidences of the disease do, however, occur in people in their 20s and 30s. Approximately half of those diagnosed with ALS live for three years or longer after their diagnosis. About a quarter of people live for five years and about 10% live for more than 10 years.
What causes ALS?
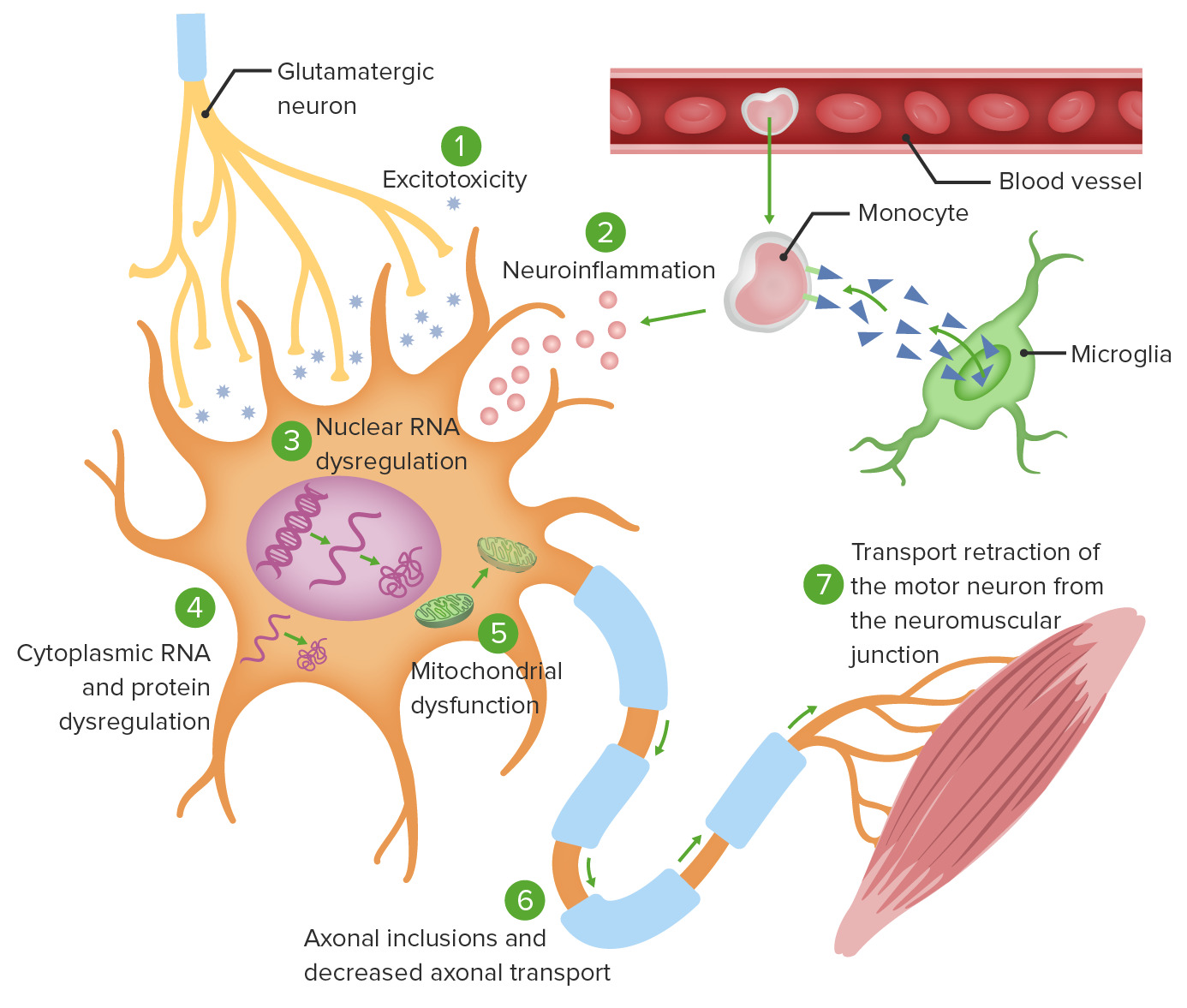
Although the etiology of ALS is unknown, recent research reveals that a number of complicated elements have a role in motor neuron loss.
Although no definitive risk factors for ALS have been established, continuing research is looking into the impact of genetics and/or environmental variables. According to research published in 2009, smoking tobacco may increase a person’s risk of developing ALS.
Anyone or more of the following factors may be responsible for the disease:
- Defective glutamate metabolism
- Free radical injury
- Mitochondrial dysfunction
- Gene defects
- Programmed cell death or apoptosis
- Cytoskeletal protein defects
- Autoimmune and inflammatory mechanisms
- Accumulation of protein aggregates (clumps)
- Viral infections
It is also likely that specific gene mutations and/or heredity modifies the disease and the likelihood of developing it.
How is ALS diagnosed?
Diagnosing ALS is difficult because there is no single medical test for it. Also, since many neurologic diseases cause similar symptoms, these other conditions must be ruled out first, through clinical examinations and medical tests. A comprehensive diagnostic workup includes most, if not all, of the following tests and procedures:
- electrodiagnostic tests includingelectomyography (EMG) and nerve conduction velocity (NCV), evaluating areas that are involved such as the bulbar region, (the head, neck and brain for speech and swallowing), as well as the cervical region (arms, diaphragm), thoracic region (muscles of breathing) and the lumbar region (legs)
- blood and urine studies, including high-resolution serum protein electrophoresis, thyroid and parathyroid hormone levels and 24-hour urine collection for heavy metals, in order to rule out any immunological or inflammatory disease
- spinal tap
- X-rays and/or magnetic resonance imaging (MRI)
- CT Scan of the cervical spine
- muscle and/or nerve biopsy
- thorough neurological examination
Individula doctors will determine which of the above tests to conduct, usually based on the physical exam and the results of previous medical tests the patient has had.
Is there a cure for ALS? How is ALS treated?
Currently there is no known cure or treatment that halts or reverses the progression of ALS. However, the FDA-approved medications riluzole (brand names Rilutek, Teglutik) and edaravone (Radicava) have been shown to modestly slow the progression of ALS. In addition, there are several promising clinical trials being conducted worldwide that are yielding important information on how to combat this disease.
While the search for effective treatment and cure continues, multidisciplinary teams across the globe are assisting patients and their families to adjust to the many challenges of living with ALS. These teams of specialists use devices and therapies to help patients manage their ALS symptoms and to allow people with the disease to maintain their independence and quality of life.
Treatments and interventions may include:
- proper body positioning
- exercise regimens, physical and occupational therapy
- devices and supports to help people walk
- braces and splints for the legs and arms
- customized wheelchairs
- home assessment to make it easier to get around in the house
- technological devices that help people communicate
- suggestions for easier-to-swallow foods and liquids
- support from a nutritionist
- feeding tubes
- diaphragm pacers
- devices to help support breathing
Many people with ALS and other neuromuscular diseases decide to take part in research studies to help test new medications and treatments aimed at treating the disease. To learn more about these studies, visit the US National Institutes of Health Clinical Trials Registry.
Learn more about ALS from the additional content below, and by visiting Hospital for Special Surgery’s ALS Program.
Has Anyone Ever Recovered From ALS? My once-vibrant husband died of ALS, and my complicated grief is deep
I remember some of our last conversations, when things were very difficult. His forewarning that this existence with him teetering at the brink of life and death was much easier than the life I would lead as a widow, raising two young children.
I think neither of us really understood that the emptiness I’d feel would be soul-crushing. That this thing they call complicated grief, in which healing doesn’t occur as it’s supposed to, and which supposedly happens only after a year, is something that I feel now. And that with a sideward glance at his frozen body I would see him looking at me; a look that was timeless and enough to convey that he loved me forever. No matter that he could no longer hold me or say it in words.
It does not help the grieving process that I am a highly functional person. In fact, I find it a betrayal of my inner broken self. drop them off at school, pick them up and be their everything; review for my internal medicine recertification board exam (no matter that it takes me a whole day to get through subject matter that I would, in my previous life, been able to complete in a half-hour); try to write scientific papers with my research team; complete the endless tasks of informing every single government body about my husband’s death; tackle rodent problem in my backyard; and yet feel completely disconnected from this world.
I wonder what he would have done if he were me.
Would he have written more scientific papers? (Probably.) Would his first paper have been about grief, or would it have been about clinical trial criteria for diseases like ALS ? (Likely the later.) I try to be my husband by nibbling on my kids’ toes or sneaking some gummy bears and Swedish fish into their snacks. (He did both). And what would he have done to be me?
I have received so much kindness. It is overwhelming sometimes. Words come pouring out of people, and I wish that I was the proper receptacle for all of these beautiful emotions. Because being open to these emotions means accepting your loss.
Words are all we have when we talk about grief, and yet they completely fall short.
I have been on the other side. I’ve talked to my patients who have lost their loved ones to cancer or heart failure or suicide about how sorry I was for their loss, that we have therapists on-hand to talk about grief, that isolation would make it worse, that routines are important, so on and so forth. It’s all well-meaning and practical, and yet, now I see, off the mark.
What I will now say to my patients who are trying to cope with grief just like I am is that no words can make this feel better. That with healing also comes loss, because with each passing day, as the acuity and rawness of the loss starts to wear off, so, too, does the memory. Even though it is so painful, that acuity and rawness keep the memory alive a little bit more than that healed memory. And that they will need to learn to live with their new broken selves. I will also unabashedly cry with them for their loss.
I know one day I will heal and my children will heal, too. My grief will no longer be complex, as I see it now. We will see Rahul come alive in every aspect of our lives. But as I mourn the life of this man who was to be my life partner, that’s almost too painful to think about.
Maya Vijayaraghavan is an internist at the San Francisco General Hospital and an assistant professor at the University of California’s San Francisco School of Medicine.